What is Female Infertility?
What is Female Infertility?
Understanding Infertility
Female infertility refers to a woman’s inability to conceive or carry a pregnancy to term. It can result from a variety of conditions that affect the reproductive system. Female infertility accounts for around 30-40% of all infertility cases.

Common Causes of Female Infertility
- Ovulation Disorders: Conditions like Polycystic Ovary Syndrome (PCOS) and hypothalamic dysfunction can disrupt regular ovulation, making it difficult to conceive.
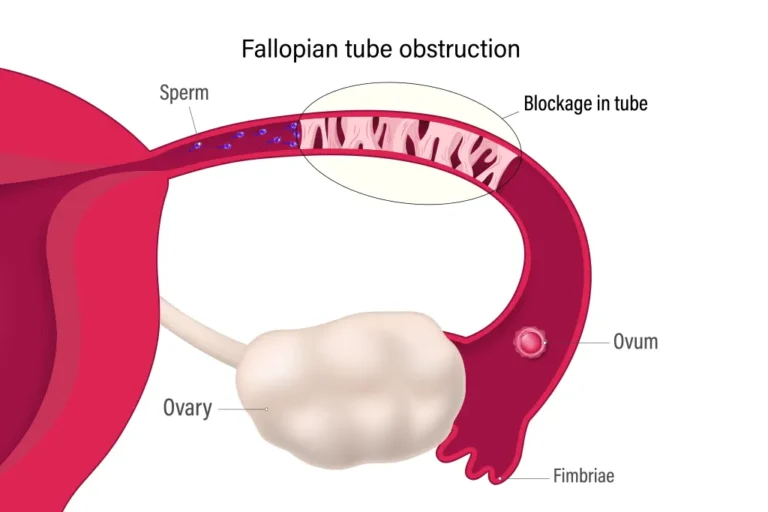
- Blocked Fallopian Tubes: Damage or blockage in the fallopian tubes due to pelvic inflammatory disease (PID), endometriosis, or previous surgeries can prevent sperm from reaching the egg.
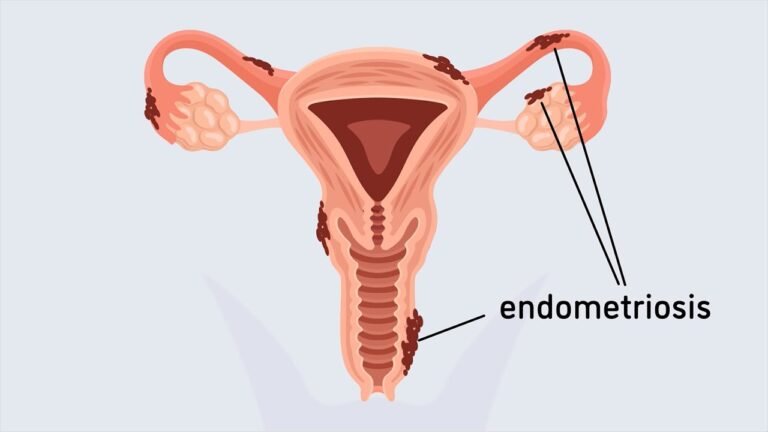
- Endometriosis: A condition where tissue similar to the uterine lining grows outside the uterus, often causing pain and reducing fertility by affecting the function of the ovaries, fallopian tubes, and uterus.
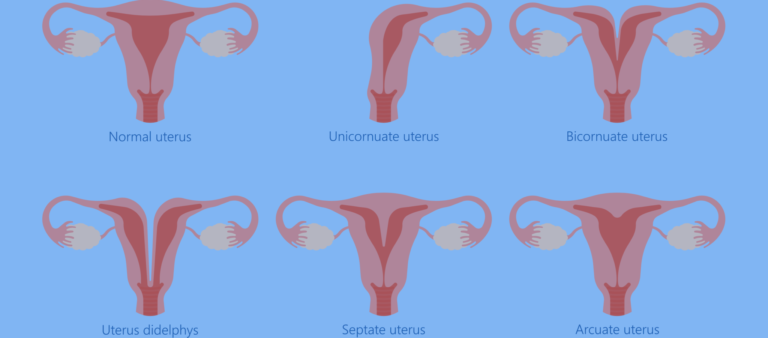
- Uterine or Cervical Abnormalities: Structural issues such as fibroids, polyps, or scarring can interfere with the implantation of an embryo.
- Diminished Ovarian Reserve: The number and quality of eggs decline with age, especially after 35, reducing the chances of a successful pregnancy.
- Annual Exams
During these exams, healthcare providers can assess various aspects of a woman’s well-being, including reproductive health, cardiovascular health, and overall physical and emotional well-being. They often include a pelvic exam, breast examination, blood pressure measurement, and discussions about contraception, family planning, and any concerns or questions the patient may have.
Here are some of the check up and health screenings that you should get done:
- Pelvic Exam
- Pap Smear (Cervical Cancer Screening)
- Breast Exam
- Blood Pressure Measurement
- Cholesterol Screening
- Bone Density Scan (DXA)
- Blood Sugar Test (Glucose Screening)
- Thyroid Function Tests
- Blood Count (Complete Blood Count, CBC)
* The specific exams and screenings recommended can vary based on a woman’s age, family history, personal health history, and risk factors. It’s essential to discuss your individual healthcare needs and screening schedule with your healthcare provider.
- Symptoms of Female Infertility
- Irregular Menstrual Cycles: A cycle that is consistently too long (35 days or more) or too short (less than 21 days) can indicate an ovulation problem.
- Painful Periods: Severe menstrual cramps and pelvic pain may be a sign of endometriosis.
- Hormonal Changes: Symptoms like sudden weight gain, severe acne, or hair loss can indicate hormonal imbalances affecting fertility.
- Diagnosis and Testing
Diagnosing female infertility involves several steps:
- Blood Tests: To check hormone levels related to ovulation.
- Ultrasounds: To evaluate the health of the ovaries, uterus, and fallopian tubes.
- Hysterosalpingography (HSG): A specialized X-ray to check for blockages in the fallopian tubes.
- Laparoscopy: A minor surgical procedure to look for endometriosis, pelvic scarring, or other structural issues.
Treatment Options for Female Infertility
- Ovulation Induction: Medications like Clomiphene or Gonadotropins can stimulate ovulation in women who don’t ovulate regularly.
- Surgery: To remove fibroids, polyps, or treat endometriosis.
- Assisted Reproductive Technology (ART): Procedures like IUI and IVF can help overcome challenges like blocked fallopian tubes or unexplained infertility. In IVF, eggs are fertilized outside the body and then implanted in the uterus.
Coping with Female Infertility
Infertility can be emotionally challenging, especially for women. Support groups, counseling, and open communication with a partner can help in navigating the stress and emotional aspects of the journey toward parenthood.
Frequently Asked Questions
What area of gynecology you treat?
What are the fees?
The pricing of women’s health treatments should prioritize accessibility and affordability, ensuring that essential healthcare services, such as gynecological exams, prenatal care, contraception, and screenings for conditions like breast cancer and STDs, are within reach for all women. Our aim is to provide fair and transparent pricing, along with options for financial assistance, should be made available to promote women’s overall well-being and equality in healthcare.
What are the risks and side effects of treatment?
what is the recovery time?
How will I feel after treatment?
Treatment Options for Female Infertility
Medications like Clomiphene or Gonadotropins can stimulate ovulation in women who don’t ovulate regularly.
To remove fibroids, polyps, or treat endometriosis.
Procedures like IUI and IVF can help overcome challenges like blocked fallopian tubes or unexplained infertility. In IVF, eggs are fertilized outside the body and then implanted in the uterus.
You’re Not Alone on This Journey
Infertility can be an emotional challenge, but support is here. Join our support groups, explore counseling options, or speak with a specialist to help navigate the stress of your journey to parenthood.