Follicular Studies
Follicular Studies
What are Follicular Studies?
Follicular studies are a series of ultrasound scans performed to monitor the development of ovarian follicles, which contain eggs. This tracking helps determine the best time for conception, whether through natural intercourse, IUI, or IVF.

Why are Follicular Studies Important?
Follicular studies help:
- Accurate Ovulation Timing: Precisely identifies ovulation timing, maximizing the chances of conception.
- Personalized Treatment: Tailors fertility treatments to individual ovulation cycles for optimal effectiveness.
- Medication Response Monitoring: Tracks response to ovulation-stimulating drugs, ensuring safety and efficacy.
- Reduced Multiple Pregnancy Risk: Controls the number of mature follicles to minimize the risk of multiple pregnancies.
- Ovarian Reserve Insight: Provides information on egg supply and ovarian health for future planning.
Follicular studies help:
- Annual Exams
During these exams, healthcare providers can assess various aspects of a woman’s well-being, including reproductive health, cardiovascular health, and overall physical and emotional well-being. They often include a pelvic exam, breast examination, blood pressure measurement, and discussions about contraception, family planning, and any concerns or questions the patient may have.
Here are some of the check up and health screenings that you should get done:
- Pelvic Exam
- Pap Smear (Cervical Cancer Screening)
- Breast Exam
- Blood Pressure Measurement
- Cholesterol Screening
- Bone Density Scan (DXA)
- Blood Sugar Test (Glucose Screening)
- Thyroid Function Tests
- Blood Count (Complete Blood Count, CBC)
* The specific exams and screenings recommended can vary based on a woman’s age, family history, personal health history, and risk factors. It’s essential to discuss your individual healthcare needs and screening schedule with your healthcare provider.
- The Follicular Study Process
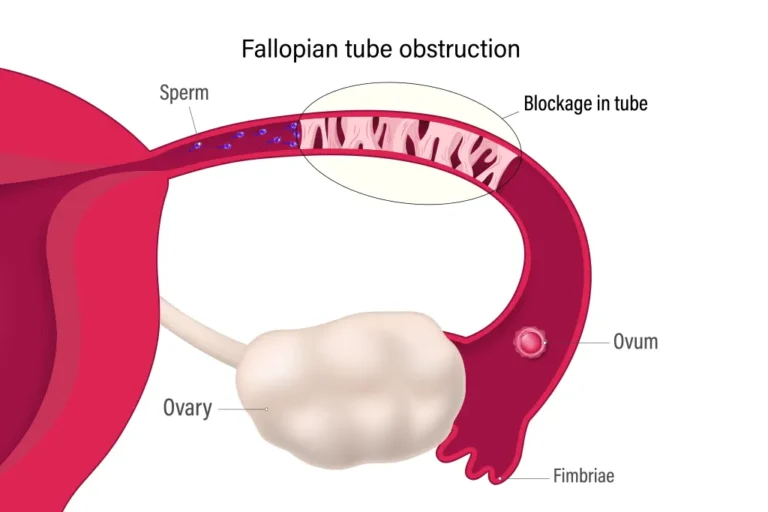
- Diagnosing Infertility Causes: When fertility issues are suspected but not identified through less invasive methods, these procedures help diagnose structural issues within the reproductive organs.
- Identifying Uterine Abnormalities: Recommended for patients with abnormal bleeding, recurrent miscarriages, or uterine fibroids or polyps to directly visualize and address uterine conditions.
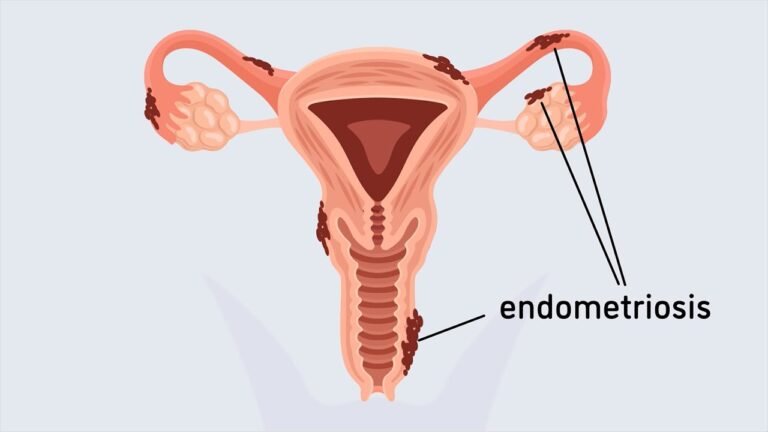
- Treating Endometriosis and Pelvic Adhesions: Often suggested for women with suspected endometriosis or pelvic adhesions that might impact fertility or cause pain.
- Evaluating Fallopian Tube Blockages: Laparoscopy can assess and sometimes treat fallopian tube blockages, which can affect natural conception.
- Unexplained Infertility: Used when other fertility tests show no abnormalities, providing a deeper look into the uterine cavity and pelvic area.
The Follicular Study Process
- Benefits of Follicular Studies
Follicular studies provide valuable insights into a woman’s ovulation pattern, helping doctors personalize treatment plans and significantly increase the chances of successful conception.
Frequently Asked Questions
What area of gynecology you treat?
What are the fees?
The pricing of women’s health treatments should prioritize accessibility and affordability, ensuring that essential healthcare services, such as gynecological exams, prenatal care, contraception, and screenings for conditions like breast cancer and STDs, are within reach for all women. Our aim is to provide fair and transparent pricing, along with options for financial assistance, should be made available to promote women’s overall well-being and equality in healthcare.